If you’ve lived with autoimmune disease for any length of time, you already know this on some level: healing isn’t linear.
There are seasons when your health feels steady and predictable, when the routines you’ve built genuinely support your life. And then there are moments that ask you to slow down, reassess, and adapt—sometimes after years of feeling well. Those moments can feel especially confusing, even discouraging, when you’ve been doing everything “right.”
In Episode 56 of the Autoimmune Wellness Podcast, I’m sharing a personal healing update after more than a decade of relative stability, including a new autoimmune diagnosis I never expected. I also talk about what this past year has taught me about stress, hormones, perimenopause, and what long-term, sustainable healing actually looks like in real life.
This post expands on that conversation and provides context for why I chose to share this chapter publicly—and how it ultimately led to a big new announcement.
.
Listen to the Episode
.
When Long-Term Stability Shifts
For many years, my autoimmune disease simply wasn’t the center of my daily life.
After my original diagnoses of Hashimoto’s thyroiditis and celiac disease, discovering and implementing the Autoimmune Protocol helped calm my symptoms and gave me a foundation I could build on. With appropriate medical care, careful food reintroductions, and routines I could actually sustain, my health became stable in a way I never took for granted.
That context matters, because what unfolded more recently didn’t come from neglect or burnout. It came after a long stretch of genuinely feeling well.
Last year, while finishing my master’s degree and writing my newest book, I experienced two episodes of uveitis—an inflammatory eye condition. When the inflammation recurred, it triggered a deeper medical workup that eventually led to a new diagnosis: psoriatic arthritis.
Rather than feeling frightening, that diagnosis felt clarifying. It helped explain patterns that had been present quietly for years, including tendon pain and recurring “injuries” that never fully resolved despite careful management.
.
Healing Isn’t About Avoiding Setbacks
One of the most important messages I share in this episode is this:
a new diagnosis does not mean healing failed.
Healing with autoimmune disease doesn’t mean you’ll never face challenges again. It means you’ve built a foundation that allows you to respond with more awareness, support, and resilience when your body asks for something different.
In my case, this season prompted deeper reflection around two major influences: stress and hormones.
The intensity of book production—especially photographing more than 100 recipes myself—pushed my physical capacity more than I realized at the time. At the same time, subtle but persistent shifts aligned closely with perimenopause, including changes in sleep, anxiety, and clear cyclical symptom patterns.
Recognizing those patterns allowed me to be proactive rather than reactive. Instead of overhauling everything or chasing solutions, I focused on observation, appropriate medical support, and adapting my routines to meet my body where it is now.
.
What My Wellness Routine Looks Like Today
After sharing a personal update like this, many people naturally wonder what my day-to-day wellness routine looks like now. In the episode, I walk through this in detail.
I want to be clear: what I share is not a template or a recommendation. It reflects my body, my history, and my current season of life.
My approach is intentionally foundational. I prioritize:
A highly personalized diet shaped through AIP elimination and careful reintroductions
Strength training and movement that supports joint and tendon health
Adequate rest, recovery, and sleep
Minimal, targeted supplementation
Working primarily with conventional medical providers, with additional support when appropriate
Just as important is what I’m not doing. I’m not chasing wellness trends, extreme protocols, or expensive “hacks.” Over the years, I’ve seen how often those approaches promise quick fixes and deliver very little lasting support. What continues to hold up—both in research and real life—are the basics, applied consistently and sustainably.
.
Why This Season Led to The New Autoimmune Protocol
This year of reflection also coincided with something else: a growing realization that the Autoimmune Protocol itself has evolved.
AIP is no longer just a patient-led experiment. It’s now supported by clinical research, used by healthcare providers, and taught through professional training programs. With the introduction of Modified AIP, the protocol has become more flexible and accessible while remaining grounded in evidence.
And yet, there hasn’t been a single, fully updated print resource that reflects where AIP stands today.
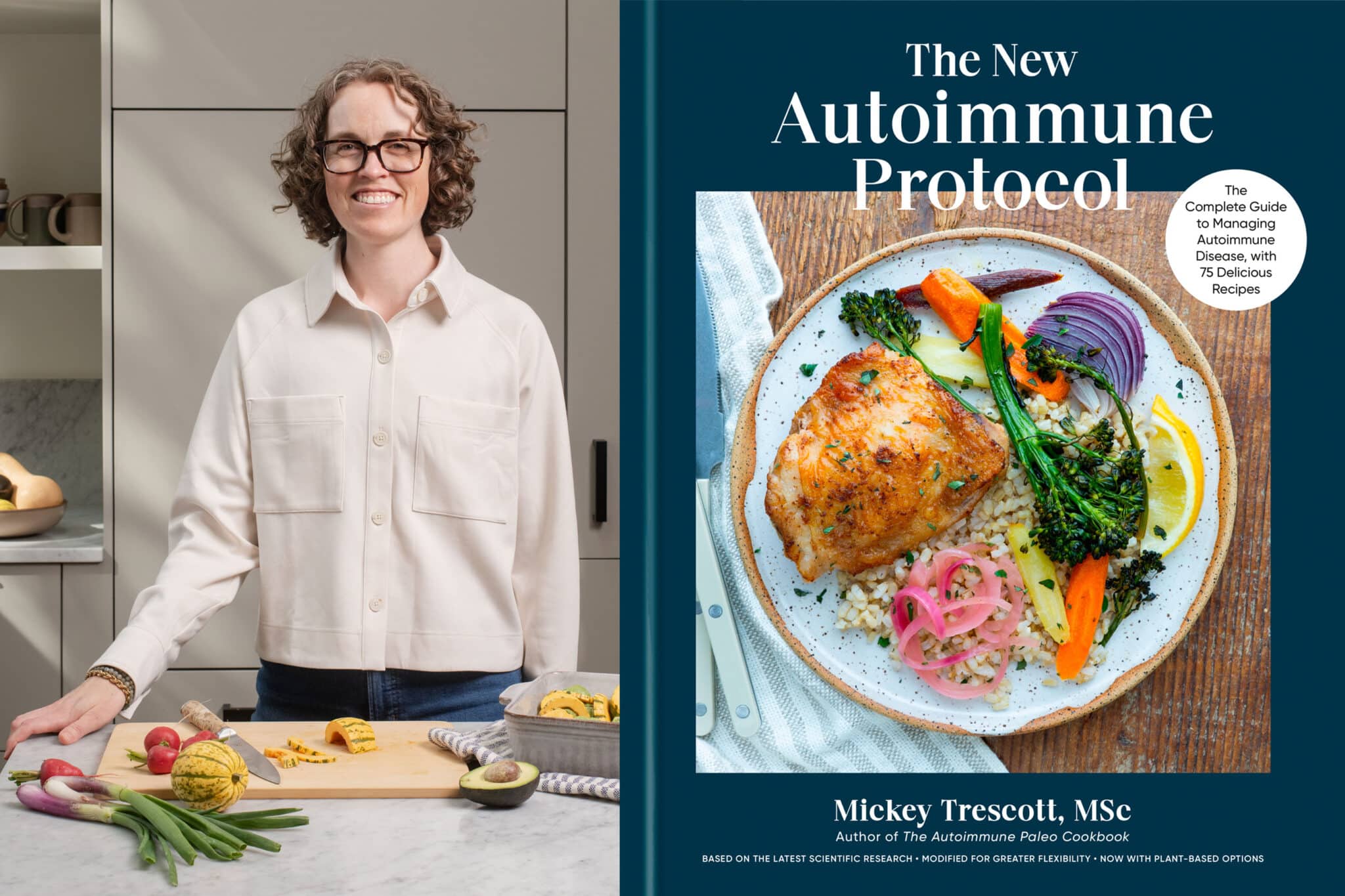
That realization became the seed for my new book, The New Autoimmune Protocol.
This book brings together more than a decade of lived experience, research, and community learning. Half of it serves as a fully updated AIP program guide. The other half is a practical, real-life cookbook designed to support long-term sustainability—not perfection.
.
Building a Foundation That Can Adapt
If there’s one takeaway I hope comes through clearly in this episode, it’s this: healing isn’t about locking yourself into a rigid plan forever.
It’s about building a foundation strong enough to adapt as your body, life, and circumstances change.
My journey has included long stretches of stability, unexpected turns, and moments that required deeper attention. Through most of it, I’ve been able to work, move my body, build relationships, and do meaningful work—not because I avoided challenges, but because I had tools to meet them.
That’s the kind of healing I want for you, too.
.
Episode Timeline
00:00 – Why healing isn’t linear & what this episode covers
02:28 – My original autoimmune story and early AIP journey
08:38 – Building strength, stability, and resilience over time
10:53 – Why ongoing support still matters
13:06 – A year of integration and reflection
15:53 – Book production and the first uveitis flare
20:50 – A second flare and the search for answers
24:13 – A new diagnosis and reframing the past
27:05 – Stress, hormones, and perimenopause
32:17 – My current wellness routine
42:09 – Introducing The New Autoimmune Protocol
46:15 – Live cover reveal event
47:14 – Final reflections and gratitude
.
Episode Transcript
Below is the full transcript of Episode 56 of the Autoimmune Wellness Podcast.
This transcript is provided for accessibility and reference.
Title: Healing Isn’t Linear: A Personal Update and Big News (Ep 056)
Mickey: For a long time, I didn’t think I’d ever need to do another personal healing update. After more than a decade of stability, these were years where my health felt predictable, supportive, and honestly not the main thing that I was thinking about, I found myself last year, right back in that unfamiliar territory of having new autoimmune symptoms, which led to a brand new diagnosis that I never expected to add to my already existing list.
At the same time, I was also in the middle of one of the most meaningful professional projects of my life, writing a book that I believe fully reflects where the Autoimmune Protocol is today.
So today’s episode is both deeply personal and hopeful. I’m sharing what’s been happening with my health, what I’ve learned moving through this new chapter, and how it’s reshaped the way that I think about healing, especially as women like me move into new phases of life.
I’m also finally getting to share a very exciting, big announcement that I have been holding close for a very long time.
Welcome back to the Autoimmune Wellness Podcast. I’m your host, Mickey Trescott, and if you’re new here, this podcast is where we explore what it actually looks like to live well with autoimmune disease, through science, lived experience, and real-world tools that support long-term health.
Today’s episode is very different from the others. I’m going to briefly take you back through my original autoimmune story, share what has unfolded over the past year, including a new autoimmune diagnosis, and walk you through what my current wellness routine actually looks like right now. Not from a place of perfection, but just sharing how I have adapted over time.
And then in the second half of the episode, I’m finally able to talk about something that I have been working on behind the scenes for a very long time. Today is the official cover reveal and announcement for my new book, The New Autoimmune Protocol, and I’ll share why I wrote it and what makes it different from anything I’ve created before.
As always, everything I share here is for educational purposes only and is not a substitute for medical care.
So if you’re in a season of transition with your health, if you’ve ever felt blindsided by new symptoms after years of stability, or if you’re curious about where AIP stands today, this episode is for you.
Let’s start at the beginning.
[00:02:28] Overview of My Healing Story
Mickey: Before I dive into what’s been unfolding over the past year, I want to take a few minutes to tell you about where my healing journey actually began. And if you’ve been following my work since the very beginning, some of this is going to sound familiar, and if you’re newer here, this will give you the context for why the Autoimmune Protocol became such a central part of my life and my work.
I first started having serious health problems around 2010 and 2011. I was in my mid twenties and on paper I was this incredibly healthy person. I was very active. I loved rock climbing, cycling, running, and I was eating what I believed at the time was a very good diet for me, I was vegan.
And then my health collapsed. I became increasingly fatigued, I developed intense body pain. I started experiencing neurological symptoms that were really scary and hard to explain. Eventually I became mostly bedridden, I was unable to work and lost my job.
At the time I didn’t have health insurance or access to consistent high quality medical care. This was a moment in time where I was between my parents’ insurance and there were no state offered plans that were affordable for the public. I didn’t have a job because I was so sick, and so I was really out of luck when it came to insurance.
I was actually paying out of pocket for conventional care, which I would muster up the courage to go to the doctor, save up the money, and then I was just told that my labs looked fine or that what I was experiencing couldn’t fully be explained.
Eventually, after a very long period of this, I was diagnosed with Hashimoto’s thyroiditis and celiac disease. And while those diagnoses gave me some answers, they definitely did not explain everything. Even after removing gluten and doing my best to follow medical advice, which was really nothing more than avoid gluten, I still had persistent symptoms that made daily life very difficult.
It was during that period that I started researching diet and I found the Autoimmune Protocol. And I want to be really clear about this, implementing an elimination diet based on AIP brought me real relief. For the first time my symptoms began to calm, I could see patterns between what I was eating and how I was feeling. I felt like I had some control, some agency in my own health again.
And at this time I also had a background as a personal chef, which meant that I was able to translate the protocol into actual food that I wanted to eat. In 2013, while I was still very much in the middle of my own healing process, I started my blog and self-published the Autoimmune Paleo Cookbook. This was the very first recipe book ever written for AIP.
At the time, I self-published it because publishers would not even return my calls. AIP was fringe, I was told that it was just way too specific, way too niche. It was not being discussed in mainstream health or medicine, and I was being incredibly public online about the fact that I was still going through it. I was still struggling. I definitely was not sharing a before and after. I was sharing my process in real time, and that resonated with a lot of people.
Even with the dietary changes, I still had a missing piece in my own journey. In 2014, I finally found a doctor that was willing to treat my thyroid disease with the appropriate thyroid replacement hormone, and that was the moment it all came together and things really shifted.
For the first time since my health crisis began, I started to have more good than bad days. For sure it wasn’t perfect, but I was functional, I could go back to work, I could think clearly, and I could participate in my life, and I was so grateful for that newfound health.
And that being said, my recovery didn’t mean that I just went back to the body that I had before. For many years after that, I had to be very cautious with physical activity. I experienced exercise intolerance when I tried to push myself and I had to relearn what movement looked like in a body with autoimmune disease.
From that recovery through about 2019, my primary form of movement was walking. And honestly, I fell in love with it. I worked up to walking an hour, sometimes up to two hours a day. I lived way out in the country, so I had these beautiful country roads to walk on. I listened to podcasts, I talked to friends on the phone, and I really let that be my foundation for exercise. This long stretch of relative stability, combined with everything I learned through AIP, became the backbone of my work, but it also became the foundation of my everyday life.
Over time, those symptoms didn’t just become manageable. They kind of faded into the background. I had more and more energy, I was able to be more productive, at this time I was working full-time writing books and working with the AIP community, coaching, working with practitioners, collaborating with researchers. I found that I could work full days, I could travel again, I could push myself a little bit with movement and do the things that I loved without constantly having to monitor how I felt or feeling like I was going to crash.
For many years, my autoimmune disease simply wasn’t the center of my daily life anymore. And that’s something that I do not take lightly. What made that possible wasn’t chasing perfection or staying in elimination forever. It was learning my body, building a personalized way of eating through careful reintroductions, supporting my thyroid appropriately, and creating routines that I could actually sustain long-term.
I share this because it’s important context for what I’m about to talk about next. What’s unfolded more recently didn’t come from a place of neglect or burnout. It came after a long, steady chapter of feeling genuinely well.
If you want to listen to the full, detailed version of my original healing story, I shared it in depth in a podcast episode back in December of 2017 called “Deep Dive with Mickey”. Fair warning, it’s two and a half hours long. But I do take a really deep approach at all of those different things that happened and how I got well the first time, if anybody is interested.
[00:08:38] Building Strength—In My Body and My Work
Mickey: Around 2019, I started to notice something new. Even though I felt really well, I began to experience neck and back pain, likely because I was in the middle of production of my third book, the Nutrient-Dense Kitchen. It wasn’t debilitating, but it was persistent, and that was a signal that something in my routine needed to change.
At the time, most of my movement was walking, like I mentioned, which I was still loving, but it became clear that my body needed more support, especially around strength and stability. So instead of pushing harder or ignoring that pain, I decided to troubleshoot.
That’s when I began physical therapy and carefully incorporating strength training, working with an autoimmune friendly coach. Shout out to my friend Beth Connor, who helped me in this department. I needed somebody who understood how to bridge that gap safely.
This was about building muscle in a way that supported my joints, my nervous system, and my energy without triggering flares or overdoing it. And because of Beth’s amazing coaching, it worked great. Gradually, my back and neck pain resolved. I felt stronger, more capable, and more confident in my body again.
And then, of course, COVID hit, and life changed for all of us in different ways, but in some unexpected ways I felt prepared. The autoimmune community, in particular, has had a lot of practice taking care of ourselves, slowing down, adapting, and listening closely to our bodies.
During that time, I decided to go back to school and pursue my master’s degree in nutrition. I wanted to deepen my understanding and better support the AIP medical research that I was deeply involved with at the time.
Physically, I felt really good during this period, I was getting stronger, I had progressed from body weight movements into lifting actual weights consistently, and I even found that I could tolerate short bouts of running again, something that I hadn’t been able to do in, gosh, maybe seven or eight years. My back pain stayed gone. My energy was steady and cognitively, I still felt sharp and engaged.
This season really felt like an expansion, I wasn’t just maintaining my health, I was actually pushing things a little bit. My body felt resilient and my work felt aligned with everything I had lived and learned up until that point.
[00:10:53] A Reminder My Body Still Needed Support
Mickey: Now during this time, I accidentally ran an experiment with my thyroid medication that ended up being a pretty big learning moment. Up until that point, I had been on the same type and dose of thyroid replacement hormone since 2014, so I had been taking a compounded T4 and T3 combination that worked really well for me for years. It was stable, predictable, and honestly not something that I thought about much anymore.
Then during COVID, there was a pharmacy related disruption, and I wasn’t able to get my medication refilled for about a month. And because I had felt good for so long, I had this very natural thought, maybe I don’t need this anymore? So I decided to just lean into it and see what would happen instead of freaking out.
And interestingly, I didn’t feel dramatically worse without it. I was still functioning and getting through my days. I was just a little more tired, especially mentally. Nothing that felt alarming or urgent, I was still able to keep up with my work. But when I finally took that first dose again after the month off, the difference was immediate, and honestly, really startling.
I realized that I had some brain fog that I just didn’t really pinpoint, and it lifted almost instantly. My thinking felt clear again in a way that reminded me just how subtle these shifts can be when they happen gradually. And, thyroid medications are complicated, i’m not going to give a full rundown here, but there are a couple components, t3 and T4. T3 is something that is not in every type of thyroid medication , but I learned in this moment that I am actually really sensitive to that daily dose of sustained release T3, and that really helps lift my brain fog and give me mental clarity and focus.
That experience was a powerful reminder for me. It reinforced something I’ve said many times. Healing doesn’t mean we no longer need support. Sometimes we need to continue something that we know supports our best health, and a lot of us who are on a daily medication, even if we understand the role that the medication is playing in our lives, we have this fantasy about just living without it. And in that moment, I learned that is actually one of the things that helps me feel my best and that I actually need it.
[00:13:06] A Year of Integration and New Ideas
Mickey: So in 2024, I intentionally took a lighter year. After finishing my master’s degree, while continuing all of my work in the AIP community at the same time, I knew I needed the space to recover, recalibrate, and let things settle.
I wasn’t burned out, but I was definitely aware that I had been holding a lot for a long time. So instead of jumping immediately into the next big thing, I focused on integrating everything that I do for my health. I rested more, I simplified my schedule, and I spent time reconnecting with the parts of my work that felt most meaningful.
At the same time, something interesting started to happen. With that mental space, I began seeing the Autoimmune Protocol differently, not as something new that needed to be built out, but as something that had matured and changed. And by that point, AIP had expanded far beyond its early days.
It wasn’t just this patient led experiment anymore. It was being used in actual medical research. Healthcare providers were teaching it, and there were now multiple studies showing benefits for conditions like inflammatory bowel disease, Hashimoto’s, rheumatoid arthritis, and psoriasis.
And earlier that year, the protocol itself also evolved. The introduction of Modified AIP offered a more flexible entry point to elimination. And the response from both the AIP Certified Coach community and the wider autoimmune community was incredibly encouraging. People were seeing real results often with less restriction and more sustainability. And yet something still felt incomplete.
While that updated protocol lived online, there wasn’t a single, fully updated hard copy resource that reflected where AIP actually stood in that moment, scientifically, clinically, and practically. And so that realization became the seed for my new book. Not because I felt this pressure to make something, but because it felt genuinely needed.
And after living and teaching AIP for more than a decade, the path forward felt clear. When I shared the idea with my agent, her response was enthusiastic. I soon signed with Rodale, who is my publisher with the Autoimmune Wellness Handbook, and honestly, a complete dream for me.
What surprised me the most was how absolutely easily the writing flowed. I’ve written four books now at this point, and I’ve never had this experience before. It came together in less than two months, just because I wasn’t forcing it. It just felt like I was giving form to everything that had been building over years of my lived experience, the research and the community learning.
And at that point, I felt deeply aligned creatively, professionally, and physically. I was energized by this work. I was proud of what was taking shape, and I was genuinely excited about what the book could offer the autoimmune community.
[00:15:53] Bringing the Book to Life—and Reaching a Tipping Point
Mickey: As 2025 began, my focus shifted from writing the book to bringing it to life. That meant developing, testing and finalizing recipes, and creating the photography that would live alongside them.
In the past, I had always worked with professional photographers on my cookbooks, even though I am a photographer myself, outsourcing that part of the process allowed me to conserve my energy and focus on other aspects of book production. This time was different, because I was working with a traditional publisher, and because of how the project was structured, I decided to photograph the book myself.
It felt exciting, creative, and honestly very aligned with how personal the book was. I also wasn’t doing it alone. I had help, but it was still a much bigger undertaking than I think I fully appreciated at the outset. To meet the deadline, I started batching the photography into long weekends. I’d spend three or four days in a row cooking and photographing often three or four recipes per day. And when you consider the book required over 100 photos, you can start to see how much sustained focus and the physical effort that was involved, especially while some of the recipes were still being developed.
This wasn’t a frantic or chaotic time. I really felt motivated and capable. And for the most part I felt well, but it was a period of extended intensity, long hours behind a camera and computer, some repetitive moments and fewer natural breaks than my body had been used to.
And on the last day of one of those long photo weekends, I woke up with this dull ache behind my right eye. It felt a lot like a headache, nothing dramatic. I assumed that it was just eye strain from working so much and decided to push through the day. By the end of the day, I noticed a red spot on the white part of my eye.
So the next morning I went to see my optometrist. She suspected episcleritis, which is a outer layer, inflammation of the eye. She prescribed a mild steroid drop and told me to use it for a few days. The redness went away, and initially it seemed like that was behind me, but within the week, the pain returned, and this time it didn’t have that red spot.
I went back to the clinic, I saw a different provider ‘because my doctor was on vacation. She said that my eye looked normal and suggested continuing the drops a little bit longer. Now, of course, things changed quickly over the weekend. I mean, why would they ever change on a weekday, right?
I woke up on Sunday morning feeling like there was this thick film over my eye. Lights had halos around them, and then the pain was just super intense. I’d taken some ibuprofen and it was breaking through. So I made plans to call the clinic first thing in the morning.
And when I did, they asked a simple but urgent question, do you have a driver? And within minutes, I was sitting in front of an ophthalmologist for an emergency appointment. She told me right away that I had severe uveitis, which is an inflammation of the middle layer of the eye, and that we needed to act immediately to protect my vision.
I was prescribed a high dose steroid drop every hour, and given permanent dilation drops to rest my eye. And just like that, I went from being in full book production mode to sitting in a completely dark room, unable to work, read, or even look at my watch screen without wanting to throw up. Because if you’ve ever had your eyes dilated, you know that feeling. If you can imagine just doubling up on that, it just is a horrible experience.
For a full week while I waited for my inflammation to subside and hopefully my vision to come back, my world narrowed dramatically. I slept, I listened to music, I caught up with friends and family on speaker phone, and I came to a complete stop, whether I was ready for it or not.
If this had happened at almost any other time, that forced stillness might have felt doable. But being so close to a major deadline and also affecting my vision, possibly permanently, which is like a very upsetting thing to happen, made it emotionally really complicated.
I absolutely could not push, I couldn’t problem solve, I couldn’t get anybody else to do that work for me. I just had to wait and let my body respond to the treatment. And thankfully, after a week of that miserable protocol, my eye responded well enough to move on to tapering. So I entered a phase where I gradually reduced the drops and I got to stop the dilation, which was the most uncomfortable part.
And of course, I asked the doctor, why did this happen to me? And I was told what many people are told after their first uveitis episode. Sometimes this happens to otherwise healthy people seemingly out of the blue, and it only becomes more concerning if it happens again. And so you can probably guess what happened next.
[00:20:50] A Second Flare and the Search for Answers
Mickey: About four weeks after that first uveitis flare, just as I was finishing the steroid taper in my right eye, I noticed something familiar. This time it was starting in my left eye. The symptoms were subtle at first, but because I had just lived through this, I recognized them immediately. There was a faint sense of pressure and just a change in how light felt. And I actually used a lubricating drop, went to sleep, and then woke up with “the pain”, and I just knew exactly what it was.
This time I didn’t wait. I contacted the ophthalmology clinic right away, and because we caught it early, the inflammation was much easier to control. I didn’t need the dilating drops and the flare resolved quickly with treatment.
But the second episode changed the conversation. Uveitis isn’t uncommon, but recurrent uveitis raises different questions, and while it isn’t linked to the autoimmune conditions I already had ,Hashimoto’s and celiac disease, it is often associated with other forms of immune mediated inflammatory disease.
My ophthalmologist recommended genetic testing for a marker called HLA-B27. This is associated with recurrent uveitis and several autoimmune conditions, including ankylosing spondylitis, psoriatic arthritis, and certain forms of inflammatory bowel disease. I was really surprised when the test came back positive, mostly because I thought that I had been tested during my original health crisis many years ago, especially because I had so many gut issues and joint pain. It’s usually included in a workup, and I just assumed that I had been tested, but apparently I hadn’t.
And I just want to pause here for a moment, because HLA-B27 is not a diagnosis in itself. Many people carry this genetic marker and never develop an autoimmune disease, but in the context of recurrent uveitis, it is an important clue.
That result led to a referral to rheumatology for further investigation. And like many of you listening will understand all too well, that referral came with a long wait, seven months to be exact. And during that waiting period, I continued living my life. I kept working, I kept moving my body, I monitored my symptoms, but I was not spiraling. Of course, I didn’t have answers, but I trusted that I was on the right path to getting them.
Interestingly, it was during this time that another piece of the puzzle surfaced at my annual dermatology appointment for a skin check, I mentioned my HLA-B27 status to my doctor, and she paused and looked back at my history and told me that the scalp condition we had been treating for years with a topical medicated shampoo was likely psoriasis and not seborrheic dermatitis, which was her original diagnosis. Knowing that someone has the HLA-B27, there’s a 95% chance that actually is psoriasis.
And I also told her that I had started getting some small patches, like smaller than a coin on my elbows and my trunk. At the time I didn’t have any to show her, but she said that definitely tracked with psoriasis. Looking back, I realized that the scalp issue had been there since my original health crisis more than 15 years earlier. It had simply just been quiet and managed, not something that demanded my attention. That was definitely an interesting piece that fell into place while I was waiting for that rheumatology appointment.
[00:24:13] A New Diagnosis—and a Reframing of the Past
Mickey: When I finally saw the rheumatologist last fall, I went in prepared to advocate for myself, but also braced for dismissal. After years of living with autoimmune disease, that expectation becomes almost automatic, and back in my history, I had seen lots of rheumatologists, and none of them were that helpful.
I was surprised to find that my appointment unfolded very differently. After taking a detailed history and performing a physical exam, my rheumatologist told me that she believed that I had psoriatic arthritis.
She confirmed that the scalp condition my dermatologist had flagged was consistent with psoriasis. She also identified subtle nail psoriasis on my nails, and she explained that recurrent uveitis, especially the pattern that I had experienced, is a known manifestation of psoriatic arthritis.
One of the most illuminating parts of the visit came when she began asking me detailed questions about my joints and my tendons. I told her that I didn’t have what I would describe as “classic” joint pain, but then she asked a lot of questions about tendon pain, specifically something called enthesitis, which is inflammation where the tendons attach to the bone.
And that’s where I had a good laugh, because suddenly a whole history made sense. Plantar fasciitis, Achilles tendonitis, patellar tendonitis, a rotating cast of quote unquote, sports injuries that never fully resolved, no matter how carefully I approached physical therapy or rest. These issues have followed me for years, beginning around the time of my original autoimmune crisis more than 15 years ago.
I just assumed that I was simply prone to tendon injuries, especially as someone who loved being active. And my rheumatologist explained that this pattern, the tendon pain without obvious joint inflammation, is actually a presentation of psoriatic arthritis. And in my case, it had likely been present quietly for a long time.
In that moment, my diagnosis didn’t feel scary, it actually felt really clarifying. It didn’t invalidate the years that I had spent learning how to move carefully or adapt my routines, and instead, it just explained why certain things had always required a little more attention and recovery for me.
And for now, we’ve taken a watchful, waiting approach. Psoriatic arthritis can be serious, it can involve the spine, but my imaging is currently clear and I am deeply grateful for that. We’re going to continue monitoring over time with the goal of intervening early if anything changes.
Walking out of that appointment, I was really grateful to have an answer, not only for why the uveitis had recurred, but I now had a name for something that had been part of my story for years. That name, psoriatic arthritis, it doesn’t take anything away from the life that I’ve built, but it simply gives me better awareness going forward.
[00:27:05] Why Now? Stress, Hormones, and a New Phase of Life
Mickey: After receiving this diagnosis, I have spent a lot of time reflecting, not in a frustrated way, but in a really curious one. For so many years, my health has felt steady. I haven’t been living in crisis mode, I wasn’t ignoring my body, and so naturally the big question that comes up for me is… why is this happening to me now?
And I don’t think there’s ever just one answer to that question when it comes to autoimmune disease, but I do have a few theories that feel important to bring up.
The first is stress. Now writing a book, especially one that is this personal and fulfilling, is really intense in ways that are hard to fully understand unless you’ve lived it. Even though this was my fourth book, I was very intentional about protecting my schedule and building in rest. There’s no denying that the photography phase pushed me to the limit.
And the second piece, this is the one that feels the most interesting to me, is hormonal. Over the past couple years, I’ve noticed subtle but persistent shifts that align very clearly with perimenopause.
I’m about to turn 41 soon, and a couple years ago, around the age of 39, I began having more difficulty falling asleep, even though I was doing all of the things that we talk about that reliably support good sleep. I’ve also noticed an increase in anxiety. Again, despite all the practices that have always worked well for me in the past. These aren’t anything dramatic. They’re pretty quiet, but they were consistent. And I do wear an Oura ring and an Apple watch, so I can see that show up in my data.
And then in conversation with a friend who also lives with autoimmune disease and experiences uveitis, she shared something that stopped me in my tracks. She told me that her uveitis flares almost always happen the week before her period, and that there’s research showing this is a common pattern. When I went back and looked at my own timeline, both of my flares began on day 24 of my cycle, exactly one month apart.
Once I saw that, I just couldn’t deny that it was a pattern. I started paying closer attention to what I now know is scalp psoriasis as well as my tendon pain. And I realized that those symptoms were also flaring cyclically. What I had previously thought of as random or situational suddenly looked hormonally influenced.
With that in mind, I’ve recently begun working with a hormone savvy doctor to address the perimenopausal component of this picture, and I’m starting with cyclical progesterone. It’s still really early, I’m literally in the second month of taking it.
I just want to be clear that I am very much in observation mode. But what I do feel is cautiously optimistic. There’s growing evidence that supporting hormone changes earlier rather than waiting until symptoms escalate, can help protect long-term health and resilience, especially for women with autoimmune disease.
And I don’t know yet what this will look like long term, but I feel good about being proactive, informed, and supported as I move towards menopause. And for me, that feels like the most aligned approach, meeting my body where it is, rather than reacting once things fall out of balance.
Right now, I am feeling truly well, despite this new diagnosis, my thyroid symptoms are still completely managed with the approach I take to eating and living, as well as my medication. It’s been about 10 months since my two initial uveitis flares. I’m grateful that even though I have the potential to have it chronically, I haven’t had another flare, and I’m prepared to intervene quickly if one crops up.
I’m also grateful to know that the issue on my scalp is psoriasis, but it is almost completely managed with my wellness routine and my topical shampoo from my dermatologist.
And I do live with that low grade tendon pain from the psoriatic arthritis, but if I’m honest, it’s only a one or a two out of 10 at my baseline. And when it does flare up, I feel like I have a good plan for adjusting and managing until it subsides. And for me, this is mostly avoiding really deep stretching, using the sauna more, lightening my activity load, and using braces when necessary.
And going forward, I’m hopeful that getting ahead of the hormonal shifts and perimenopause are going to help my immune system feel less vulnerable to autoimmune flares going forward.
Now having said that. I also want to pause for a moment and name something that I see as one of the biggest barriers to my feeling healthy right now, something that I just want to name as I know it’s been affecting me every day for a long time, and you might be in the same boat.
I am finding that any focus on health and healing right now to feel really hard with everything that is happening in the world here in the US, especially people losing access to food and healthcare. Costs keep rising, violence and instability are so present.
Even if these things aren’t happening directly to us, they affect how safe and supported we feel. I am personally struggling with this a lot. There are days when it feels difficult to focus on my own health or the work that I do in the AIP community when so much feels uncertain or heavy.
And I don’t have a solution, I’m not trying to offer one, but I just want to acknowledge it and say that healing does not happen in isolation. We’re all moving through this together, and if it feels really hard right now, in some ways, that makes a lot of sense.
[00:32:17] My Current Wellness Routine
Mickey: Okay, so I know that after sharing my story, a lot of you might be curious what my day-to-day wellness routine actually looks like right now. So that’s what I’m going to share next.
I want to preface this by saying that I’m not sharing this as a template or a recommendation. This is simply where I have landed after many years of self experimentation, learning, and careful reintroduction. It reflects my body, my history, and my current season of life.
I’ll start with food because that’s often what people are the most curious about.
[00:32:45] How I Eat Now
Mickey: I eat a super personalized diet that I discovered doing the Autoimmune Protocol nearly 15 years ago, and then refining that through very deliberate reintroductions over time. The only food I strictly avoid is gluten. That’s non-negotiable for me, I have celiac disease.
More recently I’ve actually been able to tolerate small amounts of dairy, which is really surprising. It actually happened as an accidental reintroduction, and so far I’ve done okay with some hard cheeses. I haven’t been experimenting much beyond that, especially given my history of a serious dairy sensitivity with anaphylaxis. But it’s something that I am observing carefully.
I also don’t eat a lot of eggs. They’re one of my gray area foods. They tend to give me some digestive upset. So while I don’t strictly avoid them, they’re not a staple for me.
I’m also mindful with nightshades, especially tomatoes and raw whole peppers. Very small amounts or spices don’t seem to affect me much, but since my psoriatic arthritis diagnosis, I’m paying closer attention here as nightshades can be more problematic for people with joint driven autoimmunity.
Nuts and seeds, most of them work fine with me. I still just don’t like peanuts, but that isn’t going to change. Beans are a bit of a mixed bag, even when soaked and cooked properly. They can give me gut symptoms, but I really love how they taste, and they’re really full of fiber and nutrients, so I do eat them occasionally and accept the trade off.
I tolerate grains and pseudo grains well, I eat them regularly, especially rice, quinoa, and oats to help fuel my workouts and recovery.
And I don’t drink alcohol. It just doesn’t make me feel good or support my health goals anymore, especially as I head into perimenopause.
[00:34:25] What I Prioritize Including
Mickey: Now in terms of what I actively include, vegetables are at the very top of the list. I love to eat a wide range of colorful plants, ideally from my garden, every single day. I also love eating mushrooms.
I eat a lot of seafood, primarily sardines, mackerel, and salmon. But I also rotate in other varieties and shellfish occasionally. My protein intake is moderate and varied. I like to eat a lot of chicken thighs, ground beef, pork chops, and steak, rotating in lots of different cuts.
I eat fruit every day, especially berries, kiwi, citrus, apples, pears, and bananas, which specifically are really helpful for workout recovery. I’ve never loved tropical fruits and their high fructose content bothers my gut, so I don’t eat them very often.
I also regularly eat protein oats made with pea protein, walnuts, and flax. I find that adding 30 grams of protein to an oatmeal in the morning keeps my blood sugar stable and satiates me until lunch. Plus, it is an amazing vehicle for nutrient dense nuts, seeds, and berries.
I include chicken or beef liver pate consistently, and if you’ve been following me since the beginning, you know that pate is my ride or die, I just feel so good when I am consuming it consistently. It’s the first thing I put on the menu when I’m extra stressed or feeling depleted.
Another daily habit is fermented vegetables. I have fermented carrots, cabbage, and mix in my fridge right now. I also use broth often in soup, stews, rice, and even some of my bean dishes. I love putting fresh herbs, sprouts, and avocados on almost everything.
I do drink coffee, but only decaf because caffeine just really doesn’t make my heart feel very good. And I drink a lot of herbal teas like ginger and dandelion. I also enjoy kombucha and probiotic sodas, although I’m a little skeptical of the marketing around the sodas, so I don’t really rely on them heavily. They are a really nice option at an event where people are drinking alcohol and I want to feel like I’m participating.
And lastly, I love chocolate. In fact, over the holidays I learned how to temper chocolate and make bonbons and truffles for my family and friends.
[00:36:32] Medications and Supplements
Mickey: Next we’ll talk about medications and supplements. In terms of medications, I’m on compounded thyroid replacement hormone and cyclical progesterone. And when it comes to supplements, I’m very much a minimalist. I’m actually a little bit worried about the quality and manufacturing of supplements. There’s a big risk for cross-contamination and not actually getting what you think is in the supplement, and then also the potential that taking the wrong thing can cause harm, so I’m very careful with supplements.
I do take magnesium. I take vitamin D as indicated by my blood work, usually with breaks when my levels are good. I also take heme iron when my ferritin is low. Again, I take breaks pretty often. And then more recently I added vitamin C, CoQ10 and fish oil, as those can be helpful with uveitis. I also use fiber supplements and saccharomyces boulardii occasionally, usually when my gut feels off. But for the most part, I’m pretty minimal when it comes to supplements.
[00:37:34] Movement and Recovery
Mickey: Let’s talk about movement. Getting exercise is a huge part of my life, but I have to be really intentional about it. I play pickleball four to five days a week, and this has been completely revolutionary for me from a fitness standpoint. The rally style of playing pickleball where you start and stop works really well for my body. I get these spurts of intensity, but then there’s also built in recovery.
A game only lasts 15 minutes, so it’s not super intense if you don’t want to make it. It includes that forward, backward, and lateral movement, and while it does load the tendons, I have learned how to stay within my capacity, and I’ve worked up to longer sessions gradually. As long as I respect my limits, my body has been tolerating it really well.
I also find it really social and joyful. It’s a major stress reliever for me. And if you’ve ever been around a pickleball court, you know exactly what I mean. There’s always at least one person playing in a knee brace, an ankle brace, an elbow sleeve, and sometimes all three at once, which is me, so I feel right at home.
And one big change for me since my diagnosis of psoriatic arthritis is that I no longer do yoga. And I forced myself to do yoga for years, but I have long felt that it was contributing to muscle and tendon pain. And my rheumatologist actually confirmed that it can be really hard on overstretching the tendons for those with psoriatic arthritis. So since then, I have just been stretching lightly for just about 10 minutes a day, just enough to maintain my mobility without overstretching my tendons. And that is working really well for me.
I also lift weights three to four times a week, and this is not my favorite thing to do. I’d rather just be playing pickleball, honestly, but it has been one of the most important things. Strength training completely resolved my neck and back pain, and I’ve learned that when my muscles are strong, my tendons are actually under far less strain and I can actually play even more pickleball, which really makes me happy.
I also use the sauna, and this is a traditional hot sauna about once a week. I would love to do it more, but between pickleball and my workouts, I’m already sweating a lot. I tend to use the sauna more when my tendons are flaring up and I need to replace a workout with a recovery session.
[00:39:43] A Foundational Approach to Wellness
Mickey: And that’s it for my wellness routine. I take a really foundational approach to health with autoimmune disease, and I put most of my focus on eating well, sleeping and moving with intention, maintaining healthy relationships, finding joy, and being grateful for the times when health comes easily.
You might be surprised to hear that I get most of my medical support through a conventional primary care clinic as well as specialists like rheumatology and dermatology. And I recently brought a naturopath on board to help with perimenopause. I’m not doing any sort of concierge care or functional medicine. And while I understand how supportive those models and modalities can be for some people, I just haven’t found them as helpful or accessible for me in the past.
And I want to be really clear about something else here, because I’ve been in this space for a very long time, and I have seen things come and go and in some situations even cause harm.
I am not doing expensive or time consuming “wellness hacks”. I’m not doing cleansing, fasting, parasite protocols, detoxes, red light therapy, hyperbaric oxygen, cold plunges, or whatever the current thing happens to be on social media this month. Over the years, I have watched these trends come and go.
They get packaged as breakthroughs for general health or for people with autoimmune disease. They promise so much and they almost always ask for a significant investment of time, money, or both. What I’ve seen again and again, is that very little of it actually holds up long term. What does hold up is remarkably consistent and actually supported by really high quality medical research.
Eating a mostly whole foods, home-cooked diet that supports your healing, moving your bodies in ways that you can sustain, staying hydrated, getting enough sleep, managing your stress, and working with qualified healthcare providers when medical support is needed, using targeted supplementation based on real deficiencies or specific goals and not just hype.
That approach is definitely not flashy, it doesn’t make for exciting headlines, but it is what has allowed me to live a full active life with autoimmune disease for many years. It’s also what I see working over and over again for the people that I’ve worked with and supported in this community.
I share this just because I want to give you permission to opt out of that noise if you want. You don’t need to do everything. You don’t need to chase every new trend. Most of the time, the best use of your energy is doubling down on the basics and letting them compound over time.
[00:42:09] The New Autoimmune Protocol
Mickey: Which leads me to the reason why I am spending so much time talking about the basics, what I eat, how I move, and how I take care of myself, because that is really what AIP is all about.
You already know that AIP has evolved over the years and that there’s now strong medical research behind it, which we’ll be diving into more deeply in upcoming science episodes next month.
Until now, there hasn’t been one clear, fully updated print resource that laid out the entire AIP program as it exists today from the first steps through elimination and into long-term real life sustainability.
And that’s what brings me to the other reason for today’s episode. Today I am finally able to share about The New Autoimmune Protocol, which is coming out on May 26th, and today is the official cover reveal. This book looks honestly and clearly at the current state of AIP. So what we know, what has changed and how to apply it in a way that is realistic and sustainable.
Half of the book serves as the official fully updated AIP program guide, walking you through every phase of the protocol, including the food list, the explanations, and the practical tools to help you get started. And then the other half of the book is a cookbook with collections of both Core and Modified AIP recipes.
If you followed my work for any length of time, you know that my focus has always been on recipes that are nutrient dense, approachable, affordable, and actually doable in real life without turning your kitchen upside down.
This is my fourth cookbook. And I can honestly say I am especially proud of the recipes in this one. These are recipes that I truly believe that you’re going to be making over and over again. Not just because they support your healing process, but because they fit into real life.
One example of how my thinking has evolved in terms of recipe development. In my earlier books, I often wrote soup recipes using a whole chicken. Some people love buying and handling a whole chicken, and a lot of people, I will say, many people don’t. So in this book, I asked a different question, how can I create a deeply nourishing chicken soup with simmered bones, and tender meat without requiring someone to buy and handle a whole bird?
And the answer was chicken thighs on the bone. They’re more accessible, they still create a rich, flavorful broth and it feels so much less intimidating. And that’s the kind of practical problem solving that shows up throughout this book.
The New Autoimmune Protocol is going to be released on May 26th, 2026. I truly wish this were not a podcast so that you could see the cover right now because it is really beautiful and I worked so hard on it. But you can head over to my Instagram to see the reveal.
And now I want to take a moment to talk about pre-orders because this part really matters to me. Pre-orders are one of the most meaningful ways you can support a book and an author, especially in the months leading up to publication, they signal to a publisher that there’s real interest in a book, that people care about it, that it’s needed, and that it deserves visibility, marketing support, and resources behind it.
In fact, even one single pre-order can be more impactful than multiple sales after a book is released. Pre-orders help determine how many copies are printed, where a book is placed, and how much support it receives during launch.
But beyond the publishing industry mechanics, pre-orders mean something very personal to me. This book represents more than a project. It represents years of lived experience, community learning, research, and care. It reflects what I wish had existed when I was first trying to make sense of my own health and what I know so many of you are still looking for today. And so if this podcast has supported you, if AIP has played a role in your healing, or if you believe in where this work is headed, pre-ordering the book is a powerful way to say that it matters.
I’ll be sharing a full pre-order campaign with exclusive, genuinely helpful content as we get closer to launch. And yes, if you pre-order before the bonuses are announced, you still are going to get access to everything special coming your way.
You can pre-order The New Autoimmune Protocol wherever you buy your books, Amazon, Barnes and Noble, or your local independent bookstore, i’m going to include all of the links in the show notes.
[00:46:15] Join Me Live to Celebrate the Cover Reveal
Mickey: And to celebrate the cover reveal, I want to do something that feels really familiar for those of you who have been around since the early days. I’m going to host a live event on January 31st at 11:00 AM Pacific Time on YouTube. I’ll be broadcasting live from my kitchen here in Portland.
If you are around back when I used to go live all the time, cooking, answering questions, figuring things out together, this is going to feel a lot like that. Not a bunch of polish or perfection, just some real food conversation and a chance to connect in real time.
I will be demoing a few recipes from The New Autoimmune Protocol, talking through how I think about building meals now, and answering your questions about AIP, the new updates and how to actually make this work in real life. I also want to make it just a little extra special for people that show up live. So I’ll be doing some giveaways during the event, including a one hour, one-on-one strategy and coaching call with me, along with some other fun surprises.
I will put the link to the live event in the show notes, and I would really love to see you there.
[00:47:14] Thank You and Wrap-Up
Mickey: Woo, this has been a long one. So before I go, I just want to say thank you. Sharing this episode honestly feels a lot like the early days when I was writing blog posts and sharing updates as things were unfolding. Not because I had everything figured out, but because I believed there was value in telling the truth about the process.
And I’ll be honest, it feels vulnerable to share that I have a new diagnosis, especially after so many years of feeling well. But it also feels important because it reflects what I’ve always taught about healing with AIP. Healing doesn’t mean never having challenges again. It means that you’ve built a foundation that allows you to live a full, vibrant life with autoimmune disease. One where your health doesn’t have to define you or limit what you believe is possible.
My journey has included twists and turns, long stretches of stability and moments that ask for more attention. And through most of it, I’ve been able to work, move my body, build relationships, and do work that I care deeply about.
That’s the kind of life I want for you too. If sharing my story makes your own journey feel even a little bit easier, if it helps you trust your body, advocate for yourself, or feel less alone, then choosing to be open about this is very worth it to me.
So thank you for being here, for listening to my story and for supporting me in this next chapter. I’m really grateful to have this community alongside me as this book makes its way into the world.
I’ll see you next time.
.
Join Me Live for the Cover Reveal
To celebrate the release of The New Autoimmune Protocol, I’m hosting a live event on January 31st at 11:00 AM Pacific on YouTube.
This will feel familiar to those of you who’ve been around since the early days—live from my kitchen, cooking a few recipes from the book, talking through how I build meals with AIP today, and answering your questions in real time.
We’ll talk about:
What’s new and different in The New Autoimmune Protocol
How AIP has evolved and how to apply it in real life
Practical, sustainable ways to build nourishing meals
Your questions about AIP, reintroductions, and long-term healing
I’ll also be doing a few giveaways during the live event, including a one-hour, one-on-one strategy and coaching call with me, along with some other surprises for those who join live.
You’ll find the link to the YouTube event here. I would truly love to see you there and celebrate this next chapter together.
.
















0 comments