I grew up in Southern California, a pretty typical, happy kid–I was rambunctious, loved animals, and could usually be found bossing everyone around (what can I say, oldest of four?). When I turned seven I had a birthday party with an ice cream cake; that night I ended up in the emergency room because I couldn’t breathe. It turns out, I had severe asthma, so we were given a set of inhalers and told to avoid physical activity (including P.E. and school sports!).
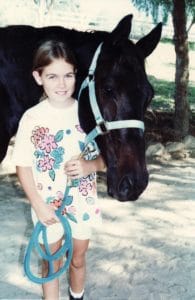
My parents, knowing this was going to be tricky with an energetic kid, decided to let me take horseback riding lessons. Riding blossomed into the perfect less-aerobic passion that combined my love of horses with light physical activity. It ended up pacifying my desire to do things like play volleyball or be on the swim team with my friends at school. I devoted hours and hours to learning how to ride, offering to do extra work at the stable and ride horses that needed exercising. This hobby turned into an absolute obsession!
Unfortunately, my asthma worsened as I grew older. My collection of inhalers continued to grow, as I needed increasingly powerful steroids to prevent the attacks. As a kid, I didn’t really stop to think about how this persistent factor in my life was affecting me, but looking back, I remember generally feeling frustrated that I could not participate in activities like most other kids. Fast forward to college. I moved to Colorado to go to school, which was a big change from the suburbs of L.A.. My asthma was a little better (can’t beat the fresh mountain air over L.A. smog!) and I was less dependent on inhalers, although I still took my daily steroid dose or I’d end up having an asthma attack. I joined a friend group that enjoyed frisbee golf, snowboarding and hiking, and was motivated to keep up with them!
Adopting a vegan diet
I was introduced to more than just clean mountain air and outdoorsy-folk in Colorado. My first off-campus apartment was with a classmate who was vegan. Before meeting her, I had never known someone who avoided eating animal products. Having grown up with a younger sibling who battled cancer and a “health nut” mom, I was used to eating broccoli and salads almost every day. But consciously avoiding animal products as an act of compassion and a move for better health was a new concept to me. It sounded great–I was all in!
A few weeks into my vegan experiment, I was talking to my mom and she asked about my asthma. I had forgotten to take my daily steroid inhaler for an entire week! She was upset, even though I said I felt fine. I told her that I would keep using it, and then promptly tossed it in the trash (like any other 18 year old would do!). I felt like I could breathe normally for the first time in my life! This realization gave me a bold idea–I could try running! Since I wasn’t allowed to run as a kid, I had never even owned a pair of running shoes. I printed out a couch to 5k program and began running in the park by my apartment. I was instantly hooked and started running five days a week. At this point I developed into an outdoor junkie–running, hiking, rock climbing, snowboarding… you name it, I was into it!
Not long after I had switched to a vegan diet, a friend of mine had a gathering and served wine and cheese. Now, historically, I wasn’t the biggest dairy fan (as a kid I refused to drink milk, eat yogurt, soft cheese, or ice cream) but I definitely had a thing for hard cheeses. That day I tried a little bite of cheese, and right away, I felt the familiar feeling of my lungs closing up and not being able to breathe… I was having a serious asthma attack. Since I hadn’t been needing my inhalers, I no longer had them, and the one for emergencies that I was supposed to carry with me was at home, creating a super stressful situation. I avoided needing to go to the emergency room, but I learned an important lesson that day – my asthma seemed to be triggered by eating dairy. Over the next few months, I would have this experience over and over again if I wasn’t careful eating at a restaurant or reading a label on a food package.
This experience deeply fueled the vegan health-kick that I was about to embark on. I had been empowered by finding out that the solution to my asthma was simply a dietary change. This led to obsessions with exercise and food. I started eating at trendy vegan restaurants, shopping for organic groceries at health food stores and loading up on new ingredients like tempeh and seitan. I ate kale, quinoa, and chia seeds, bought a juicer, and tried the raw food diet. I made smoothies full of soy protein and pomegranate juice and worked out at a gym. My friends and I regularly did the master cleanse to “clean out” our intestines. I was introduced to more people who ate the way I did and felt the way I did about health and nutrition, firmly solidifying my beliefs. And honestly, I felt great–I had loads of energy, my skin was bright, and I felt stronger and more fit than I ever had in my life.
Early warning signs
After about six months into veganism, I developed a symptom that I had never encountered before. I stopped getting my period, which had always been regular since it started (albeit late, at 16). The first missed period, I barely noticed. The second and third really got my attention. So I had my first consultation with Dr. Google, and unearthed articles about a condition called amenorrhea (loss of period). I learned this commonly happens when women lose too much body fat or exercise too much. I hadn’t lost any weight, so I thought it must be my new running habit. I cut back from 5 days a week to 3, and nothing changed, so I shrugged it off as something my body would eventually figure out. Six months later it just appeared. After that point it was always different, however– irregularity was common, my periods were much more painful than before, and I would get horrible hot flashes for their duration. I also developed cystic acne around my cycles. Now I know that I had all of the hallmark signs of hormonal imbalance. When I finally saw my doctor about this, he said that it sounded like it had worked itself out and declined to do more testing–and I was too naive to push for it.

My senior year in college I moved back to California to be near my family and boyfriend, who had moved there the year before. In the first month of school, I got engaged, and we decided to get married right after graduation. My family was having serious issues, with my parents arguing and my younger siblings all living at home and trying to navigate their teenage years with little support. This was probably the most stressful year of my life. Going to a new school, I was required to live and eat on campus, which really disrupted the good habits I had learned living on my own in Colorado (like shopping and cooking for myself). The dining hall was not vegan or fresh-food friendly, and my best meal options were salad bar with beans or tofu or a peanut butter sandwich, which I ate almost every meal of the day.
This was when I first started feeling tired. Not the kind of tired I could recover from with a weekend of good sleep–it was more of a bone-crushing tired. I didn’t make many friends or socialize at my new school. I put my head down, finished college, planned a wedding, and dealt with my family drama all the while wondering where my energy went and why I felt so terrible all the time.
After the wedding my husband and I decided to stay in California. Despite feeling low energy, this was a good time full of love, riding bikes and being outside. I drank a lot with my friends and was generally hard on my body. I had a stressful job and I would stay up late, only to leave the house in a hurry on my way to work almost every morning. I started drinking lots of coffee around this time, and got seriously addicted. On my days off I would just sleep and recover. I was still quite entrenched in veganism at this point, and was known as a really good cook by most of my friends. Even though my lifestyle and drinking made me feel horrible most of the time, I tried to make up for it by doing stints of raw diets and juice cleanses.
After a year we left California for Washington state for a change of pace. In Seattle my new friend group didn’t drink much, and over the next couple of years I realized how horribly alcohol affected me; I eventually gave it up entirely. At this point in my life, however, I felt consistently awful, and nothing I did changed how I felt. I couldn’t sleep, I started experiencing anxiety, my weight was constantly up and down, my hair started falling out, and I had even less energy than before (how was that possible?). Every once in a while I would muster up enough energy to start running, and I would only last a few weeks before I’d crash and quit. I felt like I was always on a health roller coaster.
Steady decline
In 2010, I became increasingly convinced that diet was going to fix my symptoms, and I did stricter and more severe stints of juice cleansing, like the master cleanse and raw food diets, to no avail. I started noticing problems with my blood sugar and blood pressure regulation–I would need to eat every couple of hours and despite that, usually felt like I was going to faint. I also noticed that when I’d catch a cold, I would have it for an excessively long time (like 3-4 weeks), and many times I would catch another one right on the heels of recovering from the last. It seemed as though I was sick more often than not.
One night I woke up with a strange feeling, and I woke up my husband, told him something was wrong, and then ran to the bathroom, where I passed out. My husband thought I was having a seizure because I was writhing around. When I came to, I threw up and felt like my heart was beating strangely. It was one of the scariest experiences I have had in my life. When I went to see a doctor, they said everything was fine and perhaps I had an anxiety attack. I felt incredibly upset and scared because I knew deep down something was horribly wrong with me. Why couldn’t they figure it out?

After this incident, I went back to Dr. Google, consulting the internet for ideas of what could be wrong with me. I kept encountering information about Hashimoto’s disease online, an autoimmune disease that can cause symptoms similar to what I was experiencing. Empowered by what I’d discovered, I went back to the doctor and asked for thyroid testing. All they did was test my TSH and declared me fine; even though I requested an antibody test, they refused. So I went on, going through the phases of extreme anxiety, palpitations and insomnia, alternating with phases of deep depression, fatigue and joint pain.
I repeated this cycle six times over the course of nine months–I’d get so fed up with my symptoms that I didn’t think I could last another day, I’d get an appointment with a new doctor, only to be told that my thyroid labs were normal, no they did not want to test anything further (like free hormone levels or antibodies) and perhaps I was either depressed or had an eating disorder. To be honest, I don’t remember how I got through this time feeling so demoralized and alone–I think I just put one foot in front of the other. It was rough.
Diagnosis of Hashimoto’s
In 2011, in the midst of the constant dismissal from the conventional doctors I had seen, I heard from a friend that I might have better luck with a naturopathic doctor. I found one taking new patients and he agreed to test me right away with an expanded thyroid panel, as well as thyroid antibodies and even a few other tests (like celiac antibodies). I was so relieved to finally find someone who was willing to take my concerns seriously and help me discover what was really wrong.
Not surprisingly, my TPO antibodies came back positive, indicating that I did in fact have Hashimoto’s. Not only that, but transglutaminase antibodies also came back positive, indicating that I could also have celiac disease. While I was relieved at this new information, I was completely deflated when my naturopath told me my thyroid hormone levels were normal, despite the autoimmune disease, and that he didn’t want to prescribe medication or offer any other treatment besides continuing to eat a “clean GF diet” and to do a powdered smoothie cleanse.
I was disappointed, because I was already eating tons of organic fruits and vegetables and no processed foods. As far as vegans went, I was extremely diligent about eating a varied whole foods diet instead of eating lots of processed soy and fake meat replacements. Most of the food I ate was home-cooked. I agreed to try his program, even though I could barely afford it, because I was desperate to try anything to get better.
The cleanse and reintroduction protocol
My naturopath’s protocol consisted of a smoothie meal replacement powder that was increased from one meal to three meal replacements per day, over the course of three weeks, followed by a reintroduction protocol where I then added in the commonly-allergenic foods not consumed during the meal replacement phase. I asked a friend, who practiced Traditional Chinese Medicine, to look over the ingredients. He cautioned me as the product contained a lot of harsh liver detox agents that he thought in the dose and combination, could be dangerous. I was a little worried about his take, but I decided to trust my naturopath and proceeded ahead.
I felt great while on and just after the cleanse, and actually had more energy than I had in quite some time. Unfortunately, when I made it to the reintroduction phase, I wasn’t given a lot of guidance about the procedure and I introduced many things at once. Even though the process wasn’t smooth, I discovered a lot of food reactions in this process. Soy gave me rashes and oats made my throat swell. At this point, I was afraid to eat anything but the few foods that didn’t give me a reaction. Eating became very anxiety-riddled for me. Worst yet, I felt the same level of symptoms after the cleanse that I had been experiencing before.
The crash
A couple of weeks after completing the cleanse, I started having chest pains over a few days, and ended up in the hospital with a panic attack and hypokalemia (low potassium). The hypokalemia was causing me to have muscle spasms in my chest area which were scaring me into thinking that there was something wrong with my heart. The following week, I came down with a horrible respiratory infection and was in the hospital again with respiratory distress. After I thought I had recovered enough, I went back to work, as I was worried about losing my job. Unfortunately I had to keep leaving work early as I could not make it through. This went on another couple of weeks before I was fired for coming to work sick too often.

At this point I had been suffering from unrelenting chest pain for about a month, and although the infection had come and gone, my body still felt sick and completely out of whack. I lost my appetite and 20 pounds off of my already small frame. My blood pressure was very low and I would need help getting up and to the bathroom so I didn’t fall down. I would lay on the couch all day convinced that I was dying. I lost feeling in my hands, feet, and on parts of my face and had horrible dizziness and brain fog. This was absolutely my rock bottom.
Again, I went from doctor to doctor and was tested for Epstein-Barr virus, Lyme disease, lupus, rheumatoid arthritis, and multiple sclerosis, and none of them could come up with a diagnosis except “pleurisy”, which is inflammation of the lining of the lungs. I was very anemic (low iron), and also had very low vitamin D and B12 although I had been generously supplementing all three. My grandfather, who is a rheumatologist, was speculating that I had some disease of malabsorption or that my vegan diet was making me unable to recover. I was unwilling to hear his argument, thinking that it was impossible that my diet could be contributing to my illness. Every day was a struggle, physically, mentally, and emotionally.
I had continued scouring the internet for answers since I was getting no help from conventional medicine. I consulted a specialist to be tested for celiac disease since I had positive transglutaminase antibodies. They offered to diagnose me based on the antibodies, or if I wanted further confirmation I could start eating gluten again (I had been off it for a couple of months now) and get an endoscopy. I didn’t want to do anything to cause my condition to worsen, so I declined further testing. I knew.
At this point I had been suffering from this for months on end with no relief and under great financial pressure since my husband was the only one working in our household and we had lots of hospital bills to pay off. I was extremely depressed and was trying to accept the fact that I may have to live in this condition for the rest of my life. My doctors had nothing for me, saying that perhaps I was not being careful enough about cross contamination within the home (I was being incredibly vigilant). They also told me that my symptoms could not be from my Hashimoto’s, since my lab tests were “normal”. The only treatment offered was for depression. I felt completely defeated.
Enlisting a health coach
Even though my finances were a disaster from all of the out-of-pocket healthcare expenses, I decided to give the natural route one more chance, this time with the help of a nutrition practitioner who was knowledgeable about both Hashimoto’s disease and adrenal fatigue, and was willing to work with a client eating a vegan diet. Finally, I began my slow, slow uphill journey to improved health.
At my first visit, she armed me with so much information that I felt completely overwhelmed. She suspected that a lot of my issues were related to my adrenals, and less of a direct problem with my thyroid. According to her, all of the stress and worry about my health, combined with the financial strain of losing my job and the chronic infections were taking a toll on my body. This would explain some of the bizarre symptoms I was experiencing. Our plan of action was to work on some lifestyle changes and supplementation to help nourish my system.
What I really gained from working with this coach was some hope that I’d be able to see some positive changes. The amount of time she spent listening to my concerns, and being open to the little connections I had made was shocking compared to how I had been treated by my conventional doctors. For the first time in this whole ordeal, I thought maybe I had a chance of recovering, and that motivated me though the future phase despite intense suffering.
Ending my vegan diet
My work with this coach took a long time, spanning many months of slow progress in adjusting dietary, lifestyle, and supplement interventions. One thing that was initially transformative was troubleshooting low stomach acid. She had the insight that my vitamin and mineral deficiencies, as evidenced on lab testing, were not resolving because I likely had digestive issues (I was struggling to bring up iron, vitamin D, and b12). She initiated a hard conversation acknowledging that she saw the quickest road to progress at resolving these specific nutrient deficiencies when people were willing to eat at least some animal products. Since aggressive supplementation of these nutrients wasn’t making a dent (we gave it 90 days at first), she suggested I think about trying to incorporate some animal foods for a short period of time to see if that was a part
of the issue, all while being gentle and acknowledging my nearly 10 years being vegan (this was a hard conversation and I almost fired her, but I am so grateful we had it!).

At this point in my journey, I had tried so much, and I was simply done with being sick. Although I wanted to be successful at healing while remaining vegan, I decided that I would do a trial on incorporating some animal products to see if it made a difference, and then I would make a decision on what to do from there.
I started with fish, and then eggs, and I started supplementing with digestive support to help with the transition. In the first two months of eating animal products I made some small, but noticeable gains. I started to be able to stand long enough to cook for myself and walk a couple of blocks. I continued learning about how vegans and vegetarians were often low in stomach acid because meat was the best source of the vitamins and minerals needed for HCL production. This is why so many report digestive issues after incorporating animal products into their diets again. I was surprised to find that I did not experience any digestive issues during this transition (I’m guessing because of the smart supplementation protocol my practitioner had me on!). If anything, I experienced less digestive distress than before.
While I did start feeling better in some ways, I continued to struggle with anemia (low iron, which is common with both Hashimoto’s and celiac disease). At this point, I was deep in research about diet and autoimmune disease, and I had learned how even certain cuts of meat (like organ meats) had incredible amounts of nutrients compared to others (like muscle meats), even when they come from the same animal. My reluctance to do this can’t be understated (I was extremely opposed to eating red meat), but I decided to try an experiment in incorporating first red meat in general, and then organ meat, to see if it would produce change in my iron markers.
The first red meat I ate was ground lamb, cooked by my husband with a big side of mixed vegetables. I had to be outside while he cooked it due to the smell. I ate only about a tablespoon or two, mixed in with vegetables. I went upstairs to sit in bed, expecting to be sick, but to my surprise, I felt warm and calm, and I had some color in my face. Looking for a verifiable measure of what I was feeling, I took my temperature, which had consistently been in the 94-range throughout my hypothyroid crisis. That moment, I was at 97.5. I believe my body was responding positively to the iron, B vitamins and other nutrients in that meat, and was a clear indicator that starting to eat animal products again would be a factor in my recovery. Over the course of a few months of taking the next step and eating some beef liver pate, my iron numbers climbed and climbed, normalizing for the first time on my lab work. The results were in!
Mindset shift over eating meat
It was clear to me that animal foods were offering me nutrition that was necessary to fuel my healing process, but I hadn’t completely processed the emotional side of starting to eat meat again. Ultimately, I came to the decision that my life was not worth living in suffering so that an animal would not suffer. I did a lot of reading on the topic from other ex-vegans, and how they both regained their health and found peace with sourcing animal foods that were both ethical and sustainable. I decided that I would be OK eating small amounts of animal foods, medicinally, for the nutrients I needed to recover. I would be careful about ensuring those animal foods would come from farms that took animal welfare, ethics, and sustainability seriously.
Not only did I NOT get sick when incorporating animal foods again, but I felt the first changes in the right direction. I felt like my healing was intensified as I started to eat more high-quality meat (and to be clear, I was still eating mostly plants, but with added cold-water, fatty fish, organ meats, and red meats from pastured animals). The most striking change was a mental clarity and increased energy that I had not felt in years. I was still sick, but there was no doubt in my mind that my body was responding positively to eating animal foods.
Transition to paleo and the Autoimmune Protocol
I’m a curious person, so I continued to research more about the connection of diet and autoimmune disease (especially since my result had been the opposite of what I’d expected). I searched high and low for stories on the internet of those who had recovered or were managing their autoimmune disease well on a vegan diet. I couldn’t find any–but I found a few stories talking about improvements on a Paleo-style diet, which intrigued me.

Through learning about Paleo in 2011, an ancestral-inspired way of eating that removes grains, beans, legumes, and other modern foods, I found some short references to the Autoimmune Protocol. This was an elimination and reintroduction diet that some Paleo diet researchers were encouraging those with autoimmune disease to try, based on current research on diet, nutrition, autoimmune disease, and gut health. At this time (2011) the Paleo diet was gaining in popularity, but there were no resources for the Autoimmune Protocol–these leaders in the Paleo community simply said that “based on research, those with autoimmune disease might consider removing eggs, nuts, seeds, and nightshade-family vegetables from their diet as well, and reintroduce those foods at a later time to assess tolerance.” Since I had already introduced meat and cut most grains, legumes, and dairy from my diet, I figured it was worth a shot.
Since there was no firm guideline on how to conduct this protocol, my transition to the Autoimmune Protocol was a little disorganized. Most of the eliminations came easily, but I cycled in and out of eating nuts, seeds, and nightshades, as I wasn’t sure these were going to be an issue. Around this time I met a few other women online who were also trying the Autoimmune Protocol for their respective conditions, and we banded together to support each other through the elimination phase (you can read more about the history of the AIP movement here!).
Even though I had been including animal foods in small quantities for a few months, progress was slow. That progress sped up once I gained the courage to try red meat, and started incorporating organ meats. In fact, I made so much progress in one month, as evidenced by my energy levels and lab work (I had reversed all of my major deficiencies!), that I was actually angry that no doctor had told me that I should consider changing my diet. Not only did my energy improve, but my digestion started shifting as well, meaning I could start weaning off digestive support supplements. I still had a long way to go, but I was finally making regular progress in my healing.
Back to work
At this point in my journey it had been nine months since I had lost my job due to illness, went through my crash, and spent a couple of months on a slow trajectory upward. I had racked up an impressive amount of medical debt due to two hospital stays, lots of out-of-pocket expenses like naturopathy and supplements, and long-term loss of income due to not working. Even though I was barely able to, I needed to go back to work part-time in order to make ends meet.
After putting out some good intentions and a surprisingly small search, I found a situation that was perfect for me–a family in my area needed a personal chef part-time to help prep and cook healthy food for them. They were so kind when I told them about my health challenges, and I knew it was going to be a good match, so I took the job in early 2012.
I was still very much sick and tired, but had a small window of energy every day and figured that it would be best if I started using that for work. During this time I only had energy to work, and even some days it was hard to get through–I would come home and go straight to my resting routine. My husband did an incredible job taking care of me during this time–he did all of the shopping, cleaning, and housework. I couldn’t help but feel guilty about the situation but I needed the self-esteem boost I got from being able to work, and we needed the income.
The Autoimmune Protocol
Up until this point I was dabbling with the Autoimmune Protocol, mostly because I was not sure how to overcome some implementation challenges. My healing had plateaued–although I was no longer bedridden and many of my rock bottom symptoms had improved, I was still incredibly tired and needed an excessive amount of recovery time when I got home from work.
The next phase for me was when I started reading the work of Weston A. Price and started learning about the concept of nutrient density. I started making bone broth and fermenting vegetables. I also made eating liver pate an actual part of my routine, not just an experiment. Dr. Sarah Ballantyne started writing about AIP on her blog, highlighting her thoughts on the importance of nutrient density in healing from autoimmune disease, and her work gave me the courage to really amp it up.
At this point in the history of AIP, there was no guidance about how long to do an elimination. In fact, I didn’t really know how long I’d been eliminating certain foods, since my implementation at the onset had been so disorganized. Looking back, I think I went about nine months until reintroduction, which was a lot longer than I’d recommend to most people now, but I was also dealing with some pretty deep nutritional deficiencies that needed to be reversed.
All the while, I was slowly, but surely getting better. Although I could not notice the difference day-to-day or even week-to-week, looking back on detailed symptom journals showed a clear trajectory. Some symptoms that had plagued me for many months after my crash, like hair loss and neuropathy, started going away.
Troubleshooting and Hashimoto’s treatment
Even though I had seen so much success working on my own with dietary and lifestyle changes, I was also learning about the natural and functional medicine movements, and how I may have some underlying issues that needed to be worked on with the help of a practitioner. I researched doctors in my area and one naturopathic doctor stood out from the rest in her expertise with Hashimoto’s. The only issue was that she had a 3-month wait for an initial appointment (darn!). I remember being disappointed, but resolved to continue to work on my own until I could get in to see her as it was worth the wait to see a skilled practitioner.

At this time, my biggest complaint was being simultaneously tired and sleepless. Unlike the depths of my illness, when I would easily sleep 15-16 hours a day, now I had trouble falling asleep, staying asleep, and waking up too early despite having deep fatigue and extreme tiredness. My brain felt overactive and unable to focus.
When I finally got in to see the new doctor, she ordered salivary cortisol, neurotransmitter, and thyroid testing. The results from these showed that I had a wonky cortisol curve (high in the morning and night but super low during the day), massive neurotransmitter deficiencies, and was in need of thyroid medication (what? Despite what I had been told over the years by SO many doctors?!). Gradually, she put me on two neurotransmitter support supplements (mostly amino acids) and a herbal adaptogen and lifestyle changes for the cortisol. Even though my thyroid hormone levels were the same as they had always been, she disagreed with my previous doctor’s opinions and said that my levels were classic subclinical thyroid and that she wanted me to try a small dose of dessicated thyroid medication to see if it helped improve symptoms.
After about a month of implementing and adjusting to this plan I was feeling some improvements. The neurotransmitter support was enabling me to sleep amazingly well, and I found the effects of that also solving some of my other problems. Even though previously some nights I had gotten plenty of sleep, the quality was poor and I would wake up feeling unrefreshed. With the new supplement and lifestyle routine, I was sleeping heavier and waking up energized and refreshed–something I had never felt before.
The thyroid medication was working–I felt noticeably warmer and less tired. The results of my lab work showed, however, that my TPO antibodies, which had come down considerably from the level at diagnosis, were creeping upwards. My doctor told me that some Hashimoto’s patients can actually have an increase in antibodies with dessicated thyroid medications, so we decided to try a compounded synthetic version. Over time, we determined this worked well and we worked for the next 6-9 months to adjust my dose.
Becoming a Nutritional Therapy Practitioner
In 2012, after loving the transition back to cooking for a living and wanting to expand my knowledge, I decided to enroll in the Nutritional Therapy Practitioner program which was held right in my neighborhood in Seattle, Washington. My goal was to learn everything I could about the intersection of chronic illness and dietary change, so that I could offer future work in supporting people like me who were in recovery. This was also when I started my blog, then titled Autoimmune Paleo.
The program started in the fall, and when I took it, had a monthly in-person workshop in addition to an online learning portal. I was just riveted at the quality and density of information provided through the program–but also struggled to keep up, as I still had my part-time cooking job, and my own chronic illness to manage. I remember the only thing that got me through this time was utter fascination and excitement about what I was learning, as it was showing me the exact whys of how I was able to achieve such an amazing turnaround in my own journey.
At the same time, I was still in a deep healing phase with my diet, having moved on to the reintroduction stage but not finding a lot of luck. At this point I had added in some egg yolks, nuts, and seeds, but I still found that a lot of foods were off limits for me at the time. I also continued to experience some pesky Hashimoto’s symptoms, although at much less severity than before–things like brain fog, internal trembling, neuropathy, fatigue, and coldness.
In this phase of my healing journey I was overwhelmed with gratitude. Even though I still experienced symptoms, I truly felt like I was not only able to live well with autoimmune disease, but I was endlessly excited about the prospect of sharing what I had learned to help others.
The Autoimmune Paleo Cookbook

One of my intentions in taking the Nutritional Therapy Practitioner program was to gain a foundation of knowledge to eventually produce a cookbook (my favorite job had been working as a personal chef, and I wanted to put my cooking skills to good use!). In 2013, that dream came true, as I self-published The Autoimmune Paleo Cookbook first as an ebook, and then as a hardcover book the following year (you can read more about my journey publishing this book here!).
My offering, The Autoimmune Paleo Cookbook was the first-ever cookbook completely devoted to AIP recipes, and a complete labor of love. I enlisted the help of my family, friends, and even involved the support of the growing AIP community for crowd-funding after my concept was declined by publisher after publisher.
A lot of people don’t know that I wrote this book while still in the middle of my healing journey. I felt strongly that sharing my story and my recipes, despite publishers telling me it wasn’t marketable or too specific, was the best way to build an authentic community around living well with autoimmune disease.
Three years into healing
2014 was the year I really felt “settled” in my healing (you’ll notice I don’t use the word remission–more on that in a bit). Up until this point I was still experiencing occasional flares and setbacks, interspersed with periods of deep healing. This was the year I felt really strong in a way I hadn’t in a long time; I was able to drive cross-country on a 3-month road-trip to support the hardcover release of my cookbook, which felt unexpected and amazing!
I was also stable on my medication dose, and generally feeling productive and happy. I no longer needed to rely on many supplements for digestive or nutrient support. I also started to be able to tolerate more (but still gentle!) exercise, like walking, light hiking, and yoga. At this point, I felt far healthier than the couple of years preceding my health crisis. This time, I knew how to truly care for myself and nourish my body, and I hoped not to regress to that point ever again!
In 2015, I was able to travel internationally as I visited Australia and New Zealand to promote the metric edition of my cookbook. I partnered with Angie Alt to create Autoimmune Wellness, a site devoted to helping people live well with autoimmune disease, and out of our work there we started The Autoimmune Wellness Podcast and wrote The Autoimmune Wellness Handbook as further resources for the community.
The Nutrient-Dense Kitchen

As the AIP community grew and expanded globally (you can read more about the history of the AIP movement here), I began to notice that some parts of the Autoimmune Protocol were increasingly misunderstood, the primary one being nutrient density.
Since a focus on nutrient density was a big factor in reversing my nutrient deficiencies and continuing to maintain good health with autoimmune disease, I decided that it would be the focus of my next book as an encouragement to the community to keep this aspect in sharp focus.
In 2018 I began work on The Nutrient-Dense Kitchen, a cookbook that not only included a recipe collection focused on the most nutrient-dense, healing ingredients, but also provided information and actionable strategies for increasing nutrient density in the diet. I self-published it in March 2019.
Ten years into healing
As I update this story, it is the year 2021. It has been 10 years since my health crisis. I still get questions and comments on my story from readers asking how I feel now, or if I still experience autoimmune flares
In general, I have experienced very few Hashimoto’s flares since 2014 and have been stable on the same dose of thyroid medication since that time. In 2018, I experienced a major flare following a 3-week vacation to Europe (not only was I exposed to a bunch of foods I don’t usually eat, but I was very active and my rhythms were quite off). This lasted a few months, and I was able to work out of it by focusing on the foundations of sleep, stress management, and eating well. Since then I’ve been pretty stable in my healing and feeling great.
As far as how I eat today, I eat a customized, nutrient-dense diet that I have determined works for me through many years now of experimentation and the elimination and reintroduction phases of the Autoimmune Protocol. I eat lots of colorful, organic fruits and vegetables, grass-fed or pastured meats (some raised at home on my family’s farm!), organ meats, fish, shellfish, and fermented foods. Some reintroductions I tolerate well are white rice, pastured eggs, some nuts and seeds, and some nightshades (like potatoes). I have not been able to reintroduce dairy or other nightshades, like tomatoes.
I still take the same dose of synthetic compounded thyroid replacement hormone that I’ve been on for over 7 years. I take very few supplements. Over time, I continue to be amazed at the power of nutrient density and supporting the body’s digestive process and capacity to heal.

Even though I rarely experience many symptoms of my autoimmune diseases, I never use the word remission to describe the health I’ve achieved (if you want to read more on this topic, check out the article I wrote titled Why the words “remission” and “cure” do a disservice to the autoimmune community).
Every day I am filled with gratitude for the ability to have a fulfilling career, engage with those I love deeply, and do things that bring me joy. Sometimes those are a product of experiencing better health, but I’ve realized that often I can still live my dreams (sometimes with modifications), even when I’m not feeling my best, as with autoimmune disease, sometimes we have to be flexible and adaptable! I hope that sharing my story here has provided inspiration, encouragement, and an acknowledgement that healing isn’t always linear, perfect, or predictable.
















8 comments
Hello Mickey,
I am so grateful to have found your website. I have been floundering through my celiac diagnosis for 13 years (even though I adhere to a strict GF and now DF diet) and have experienced so many of the AIP symptoms. I started the AIP “lifestyle” two weeks and have been searching for answers and practitioners for past 6 months. I feel like I’ve hit the payload here. You can’t imagine how happy I am that you’ve helped me with my mindset in realizing this isn’t going to just be a diet that I check out for 6 months or so, but that it is a lifestyle that I will be eventually be embracing wholeheartedly. Also, I appreciate you for changing my mindset from one of restriction to nutrient density. These two things are making all the difference for me.
So grateful for you and Angie sharing so many rich stories and making them available through your blog and website. Can’t wait to read your books that I’ve ordered.
Susan
Thank you Susan, for your kind words here, and wishing you the best as you navigate your own recovery!
Hi Mickie and Angie,
I have been following your website for some years now, having autoimmune issues myself, and I really appreciate all the very balanced information you make available. I had never read your background stories until this morning, and having just read them wanted to thank you both for sharing them – they are inspiring and living confirmation of the importance of diet. You make a difference, thank you!
warm regards,
Linda
Hi Linda! Thanks for the kind comment, and wishing you wellness on your journey!
Hi Mickey,i am in your same situation thank u for your advices.can you tell me if u drunk wine when u where vegan?and in your aip transition you consume wine white or red?thanks
Hi Mary! I have never been much of a wine drinker, I’m sorry! I recommend avoiding alcohol during the transition and elimination phases, and potentially introducing small amounts later if it works for you. Good luck!
Hi Mickey, I just started my AIP diet last week. I have Grave’s disease. I am wondering if this AIP diet is beneficial for Grave’s disease. I have been reading a lot of Hashimoto’s disease here but almost none for Grave’s disease. I also have tried some of your recipes and they are delicious.
Thank you.
Kind regards,
Chandra
Hi Chandra! Wishing you luck on AIP. Graves’ is a lot less common than Hashimoto’s, which is why you see less stories about it being helpful, but they are out there! Nicole of Heal Me Delicious has Graves and writes about her experience on her blog: https://healmedelicious.com/about/. Good luck!