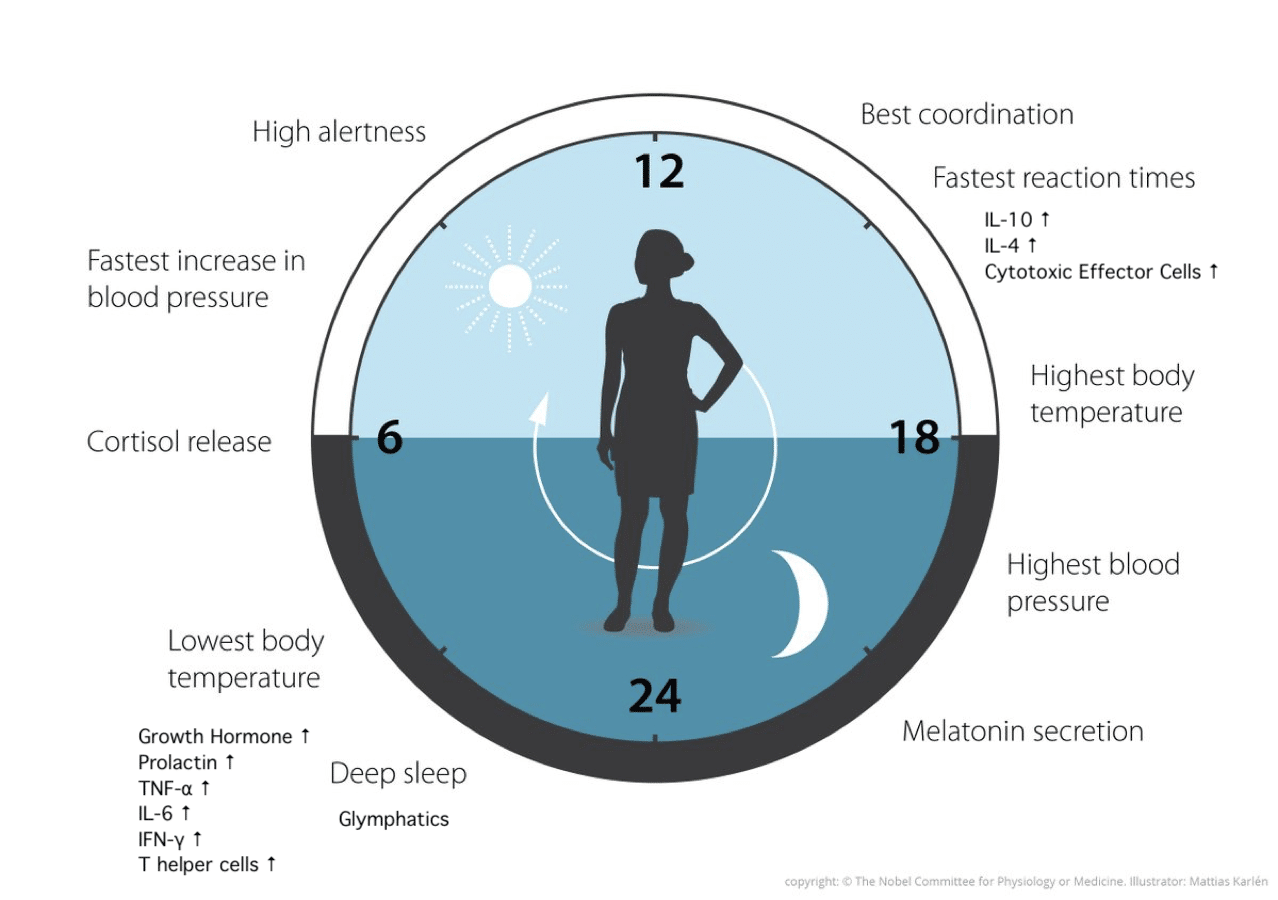
Just like clockwork, as the sun sets and darkness arrives, certain squads begin their patrol, looking for the enemy and confirming that the perimeter hasn’t been breached. No, this is not a military spy thriller. The clockwork is the ticking of the circadian clock, a rhythm of the sleep-wake cycles regulated by the solar day of 24 hours. The squads are the cells of the immune system on patrol, looking for bacterial, viral, and fungal invaders as well as errant cells. In this article I will be sharing with you why sleep is so important to your immune system and how to optimize sleep time to support your health.
What Goes on Inside Your Brain When You Sleep
Before we talk about sleep and the immune system, let’s have a refresher on the sleep stages. I know, I know, not the sexiest topic, but this is important information to understand so you can recognize in your own body whether you’re getting good sleep, and how to improve if you’re not! Grab a cup of something, roll up your sleeves and dig in!
Nomenclature used for the sleep stages varies. For simplicity, I will use the sleep stages used by many consumer sleep trackers such as Oura, FitBit, Garmin, and Whoop, so that I can use my own sleep data to illustrate. In sleep literature, you will see the terms NREM (non rapid eye movement) which encompasses both light sleep and deep sleep/slow wave sleep with four stages, and REM sleep (rapid eye movement sleep) used.
Consumer sleep trackers break sleep into four stages: awake, light, deep, and REM stages. Awake time is time spent in bed before falling asleep and brief awake times during the night, shown as white bars in my Oura ring data in Figure 1 [1].
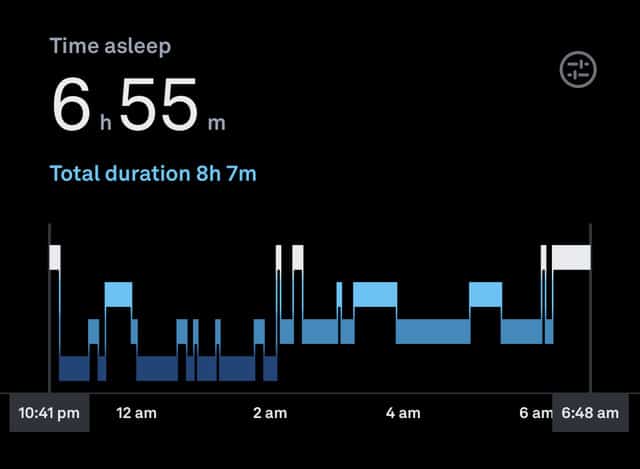
During the light sleep stage, shown in bright blue bars in my Oura ring data, your muscles relax and you may be startled by muscles jerking. Your breathing slows, heart rate decreases, body temperature drops. Waking up is easier during the light sleep stage [1].
During the deep sleep stage, also known as slow wave sleep and shown in darkest blue, blood pressure and body temperature drop and the brain flushes waste through the brain’s glymphatics system. This system, similar to the lymphatics system throughout the rest of the body, was only recently discovered and reported in 2012 due to new imaging techniques [2]. The body promotes tissue, muscle and bone growth and repair during this time by increasing blood flow and release of growth hormone. Waking up is more difficult, and you are disoriented or groggy if disturbed during deep sleep [1].
The timing of deep sleep is important. It occurs during the first half of the night. That timing is programmed by early sun exposure in the morning. If you are routinely missing the sleep bus at 10-11pm and staying awake until 1-2 am, you can be getting less deep sleep than your brain requires. The glymphatics system is the functional waste clearance for your brain and spinal cord. This clearance occurs during deep sleep by the expansion and contraction of the brain extracellular space. During this window of sleep, the brain clears neurotoxic metabolites such as β-amyloid protein as well as distributes compounds such as glucose, hormones, amino acids and lipids. Inadequate clearance of these neurotoxic metabolites may play a role in neurodegenerative diseases such Alzheimer’s and Parkinson’s disease, decades before symptoms are severe enough to be diagnosed (reviewed in [3]).
The REM sleep stage, shown in intermediate blue, is when your mind is re-energized. The bulk of it occurs in the latter half of the night when you are more easily awakened. Breathing increases, heart rate increases and vivid dreams may occur. Your body becomes immobile to stop you from elbowing your sleeping partner while dreaming. Memories are formed during the REM sleep stage, learning is cemented and those eureka moments occur helping you to solve problems from earlier in the day [1].
What Controls the Stages of Sleep? Circadian Rhythms
Now that we’ve established the sleep stages, what controls them? Circadian rhythms are regulated by light exposure and darkness through the suprachiasmatic nucleus (SCN) inside the brain. The SCN, in turn, regulates the clocks inside of each tissue, organ and cell (reviewed in [4]). Every organ has a clock which regulates cyclical hormone secretion. For example, serotonin, your feel-good hormone, is influenced by the amount of sunlight you get each day. Serotonin is later converted to melatonin which prepares the body for sleep. Melatonin supports the immune system, blood pressure, decreases accumulation of plaque in the brain, improves thyroid function, improves insulin sensitivity and weight loss. The circadian rhythm has an impact on every system of the body, including the immune system (reviewed in [5]).
How Does Your Sleep Impact Your Immune System?
The immune system is classified into two systems: the innate immune system (monocytes, neutrophils, natural killer cells) and the adaptive immune system (T and B cells). Soluble mediators, called cytokines, that travel throughout the body regulate the function of immune cells and others. The immune system is also regulated by the neuroendocrine system in an elaborate cross-talk of soluble mediators such as prolactin, serotonin, melatonin, cortisol and epinephrine [6].
We know from both personal experience, anecdotal studies, animal models and several human studies that sleep impacts immunity. Several nights of poor sleep will increase my autoimmune symptoms. We have all experienced that hard stressful push to complete a project and once it’s completed, we get hit with a bad cold or flu. We also know that an immune response to infections can impact sleep, either promoting more sleep or disrupting sleep. If you want a glimpse of what is happening with the immune system while you are sleeping, which I hope will motivate you to have sleep as a priority, keep reading.
Two hormones, growth hormone and prolactin, are at their highest during the sleep phase and have a profound impact on the immune system. Certain pro-inflammatory cytokines such TNF-⍺, IL-6, and IL-12 are highest during early sleep, which promote more cellular responses. Other anti-inflammatory cytokines are highest during the wakeful periods such as IL-10 [7].
What do these patterns mean for the functional immune system? Remember the adaptive immune system? It is composed of several sub-groups, two of which are the T-helper 1 (Th1) cells which are focused on cell-mediated responses and the T-helper 2 (Th2) cells which are focused on antibody-mediated responses. These adaptive immune sub-groups depend on other cells such as monocytes to bring the gossip, bits of proteins from bacteria and viruses, about the outside world to the local bar. The local bars are the lymph nodes throughout your body. The gossip is the presence of bacterial, viral, and fungal invaders. Lymph nodes are like going to a crowded bar at midnight and speed dating. It’s a noisy, volatile, pro-inflammatory place requiring those inflammatory cytokines TNF-⍺, IL-6, IFN-ɣ and IL-12 that increase during deep sleep. These interactions during deep sleep are required to keep the immune system in check and balanced to minimize allergies and autoimmunity. These interactions take place at night in the bars, aka lymph nodes, because there is different work to be done during the waking hours to locate and destroy the intruders, bacteria and viruses. During the waking hours, cytotoxic (killer) cells are most active presumably to protect the body from infection when we are most likely to encounter bacteria, viruses, and fungi [8].
The Proof is in the Studies!
One hundred sixty four brave souls signed up to be intentionally infected with a cold virus after monitoring their sleep patterns for 7 days using wrist actigraphy (monitors movement) and self-reported sleep efficiency. Sleep duration of less than 6 hours was the only factor that correlated with onset of cold symptoms [9]. You don’t want to get the latest cold? Make sure you are getting 7hrs of sleep AND that you are promoting deep sleep with a cool and dark bedroom with a regular bedtime.
In another study, healthy, college aged volunteers were extensively assessed for normal sleep patterns and insomnia. They were tested for antibodies to the flu vaccine before and after vaccine administration. The insomnia cohort had lower baseline antibodies from prior exposure to flu strains as well as a reduced antibody response to the flu vaccine [10]. Similar findings were observed when looking at HepB vaccination, which is a three-dose vaccine process to a novel antigen, unlike the Flu vaccine study. Shorter sleep duration had reduced antibody response after the 2nd and 3rd vaccination as well as lower clinical protection scores at 6 months post-vaccination [11]. These types of vaccine studies allow us to see functionally how the immune system is impacted by sleep.
How Does Insomnia Impact the Immune Response?
How does insomnia impact the immune response, as perceived by anecdotal evidence of more illness when sleep deprived as well as more chronic disease in those suffering with insomnia for long duration or in shift workers? Sleep is thought to be the time when daytime experiences (encoding phase) is consolidated into memories and learning. In the same way, exposure to environmental stressors and pathogens while we are awake, is consolidated into immune memory while we sleep. Just as lack of sleep impacts our ability to learn and retain memories, lack of sleep also impacts the immune system’s ability to learn from the day’s environmental exposures as well as combat current infections. Lack of sleep also exacerbates immune system imbalances such as asthma, allergies, and autoimmunity [8].
How to Optimize Sleep?
What does all of this mean for the autoimmune community? Keep sleep hygiene as a top priority in your self-care, ensuring both quantity and quality of sleep. This is critical to managing autoimmune disease to keep the immune system functioning optimally as well as for brain health. Aim for at least 7 hours of sleep each night, with consistent bed and awake times. Given the importance of deep sleep for glymphatics clearance of neurotoxic waste as well as proper interaction of lymphoid cells within lymph nodes during sleep, focus on quality sleep between 11pm and 3am. To help with deep sleep, make sure your bedroom is not too hot. By far, my sleep tip that is most successful with clients is lowering the bedroom temperature or using any of the bed coolers on the market such as Chilisleep. On average, 64-69F is the sweet spot for deep sleep but if you’re used to very warm temperatures, decrease the temperature slowly over several weeks so as to not exacerbate autoimmune symptoms.
My second most successful sleep hygiene tip is that a great night’s sleep starts in the morning. Yes, in the morning! Remember the suprachiasmatic nucleus? It receives light information from your eyes that sets the clock for your bedtime [4]. Shortly after waking, aim to get 5-15min of sun exposure, preferably outdoors but a window will suffice if needed. In the evenings after the sun has set, dim your household lights and use blackout curtains or a sleep mask if outside lights disturbed your sleep. Be sure to silence all electronic devices and if possible, remove them from the room. Above all, make your bedroom your sleep sanctuary. It should be a place of peace and serenity. No paying bills in bed. Keep your nightstand relaxing and clear. While pain can interfere with sleep, poor sleep can also increase your pain. Please speak with your medical professional about pain management and investigate methods, for example, body pillows, to help you sleep more comfortably. Keep sleep a priority as part of your self-love routine and your body and mind will thank you for it.
References
- Sheth, S., Godwin, J. Kryder, C. “What Are the Stages of Sleep & What Does Each Stage Do?” The Pulse Blog, 2 June 2021, https://ouraring.com/blog/sleep-stages/.
- Iliff, Jeffrey J., Wang, M., Liao, Y., Plogg, B., Peng, W., Gundersen, G., Benveniste, H., Vates, G., Deane, R., Goldman, S., Nagelhus, E., Nedergaard, M. (2012) “A Paravascular Pathway Facilitates CSF Flow through the Brain Parenchyma and the Clearance of Interstitial Solutes, Including Amyloid β.” Science Translational Medicine, 4(147), 1-11.
- Jessen, N.A., Finmann Munk, A.S., Lundgaard, I., Nedergaard, M. (2015). The Glymphatic System: A Beginner’s Guide. Neurochem Res 40(12), 1581-1586.
- Albrecht, U. (2012). Timing to Perfection: The Biology of Central and Peripheral Circadian Clocks. Neuron, 74, 246-260.
- Irwin, M. R. (2019). Sleep and Inflammation: Partners in Sickness and in Health. Nature Reviews, 19, 702–715.
- Bryant, P.A., Trinder, J., Curtis, N. (2004). Sick and Tired: Does Sleep Have a Vital Role in the Immune System. Nature Rev Immunol 4, 457-467.
- Lange T, Dimitrov, S., Ferm, H-L, Westermann, J., Born, J. (2006). Shift of Monocyte Function Toward Cellular Immunity During Sleep. Arch. Intern Med. 166, 1695-1700.
- Lange, T, Dimitrov, S., and Born, J. (2010). Ann. N.Y. Acad. Sci. 1193, 48-59.
- Prather A.A, Janicki-Deverts D, Hall MH, Cohen S. (2015). Behaviorally Assessed Sleep and Susceptibility to the Common Cold. Sleep. 38(9), 1353-1359. doi: 10.5665/sleep.4968.
- Taylor, D.J and Kelly, K. (2017). Is Insomnia a Risk Factor for Decreased Influenza Vaccine Response? Behav Sleep Med. 15(4), 270–287. doi:10.1080/15402002.2015.1126596.
- Prather, A.A, Hall, M., Fury, J.M, Ross, D.C., Muldoon, M.F., Cohen, S., Marsland, A.L. (2012). Sleep and Antibody Response to Hepatitis B Vaccine. Sleep. 35(8), 1063-1069.
















8 comments
Thank you for this! Any advise for this night shift nurse with RA?
Marie, how many nights in a row do you work? Which shift do you work? The 3-11pm shift is the easiest to maintain a regular schedule. It’s easier to minimize eating after 8pm and then go right to bed without eating when you get home. If you are working through the night and sleeping most of the day for many days in a row, it’s best to just pretend your awake time is day time.
Wow! This is an amazing article! Thank you so much, Sybil, for writing this! I have always known sleep is important, but to see WHY it is important really is eye-opening!
Thank you, MandyB! Yes! Change is so much easier when we understand the WHY. It makes the HOW easier to do.
Thank for this! I am navigating another MG crisis. Not had one in 3 years. Your article is a great reminder to us all and you show the science behind it. Much Thanks Friend!
Joy
Thank you for this invaluable information and wealth of knowledge about immune health. It’s our first and best offense and defense to a healthier, longer life.
I would love to be able to e mail this article to my daughter. She has terrible sleep problems. She is not on social media, so unable to share that way. Was not able to copy/paste.
Hi Kris! I would grab the link in your browser, and copy/paste into an email to send to her. Hope that works!